Sometimes several stray disparate thoughts come together and have a party in my mind and won't leave until I try to make sense of how they may relate to each other by writing them down.
Anything I've ever read about how the brain works, I come away with an image of how the brain never is still, how it waves like the ocean, has currents, states of activity that although they may vary, never actually cease.
Until we die.
And anything I've ever read about consciousness is how it fluctuates, dims and brightens and dims again, naturally, all by itself, about every 90 minutes or so. This pattern is also seen in sleep studies.
So, bear in mind, this is where I am coming from in this post: I see my conscious awareness of myself as a self floating like a bit of flotsam in an ocean of brain activity. I do not regard my brain as belonging to me: instead, I see my"self" as belonging to it.
.....
BRAIN ASYMMETRY AND NEUROTRANSMITTERS
I have a book open at all times, even if the only time I ever read a hard copy book is in the bathroom. I do not use a smartphone while in there.
It has taken me ages to read through "No Self No Problem" by Chris Niebauer, but I got all the way through it and decided to read it again. It's a short small book, paperback, easy to pick up and lay face down again without closing it. Does not take up a lot of counter space.
Good thing I decided to re-read it:
On page 50 he writes (in chapter 3 about pattern-seeking); "There is some evidence that neurotransmitters affect our pattern-perception capability. Because of this, it is important to note that the two sides of the brain differ in terms of their neurochemistry." He points to a reference, Tucker 1984. So I looked up the reference: Tucker, D. M., & Williamson, P. A. (1984). Asymmetric neural control systems in human self-regulation. Psychological Review, 91(2), 185–215.
Whoa. This was news to me. Totally missed that first time through.
To continue, page 50: "The left brain is dominant for dopamine, whereas the right brain is dominant for serotonin and norepinephrine. There are many functions associated with dopamine that range from the euphoria of falling in love to the movements of the body. Since the 1950s it has also been thought that schizophrenia is the result of too much dopamine. One of the hallmarks of schizophrenia is seeing patterns that are not there, that is to say, hallucinations."
I immediately thought of Anil Seth's TedTalk about the predictive brain and the software he used to simulate hallucination.
I put the Tucker and Williamson title into google scholar, papers since 2017, and found this nice gem: Large-scale neural networks and the lateralization of motivation and emotion. There are many more, over 6000.
All this echoes what I gleaned ages ago from reading A.D.Bud Craig's work on lateralization of interoception. I took detailed notes from a video in which he explained to a group of Swedish neuroscientists about laterality and brain function. Please read through my notes, or just watch the video. So informative!
It also echoes a recent journal containing articles all about interoception and self.
...................................................
WHAT ABOUT PAIN?
Pain is known to rob people of their sense of self.
So, I wonder, what if pain is about some weird deficit of some neurotransmitter, maybe just on one side, which would normally just inhibit pain naturally, but if it's not there, it's like a window, the blinds of which block out blaring sun have been removed? What if pain is not a "thing," but rather absence of some "thing"? Some veil that should be there so we do not have to experience too much of our own interior milieux? Our own interoceptive sensory input?
I learned a long time ago that the brain was full of inhibition, that in fact what it mostly does is inhibit itself. One side inhibits the other side and vice versa. Both sides rostrally inhibit brain parts that are more caudal. A great big inhibition machine. [NOTE: Back in here today with an edit, something I forgot to mention yesterday - if this is true, then this might be why SRIs (serotonin reuptake inhibitors) help with pain... and might have something to do with that idea about the right brain being dominant for serotonin. Maybe SRIs help the right brain inhibit the left brain better. Just a thought, and very undigested at this point, but might have something to do with something.]
I remembered Robert Sapolsky discussing POMC, the precursor molecule that is terribly scarce, made by only a few cells somewhere in the hypothalamus or somewhere, so it's "expensive" from a neurotransmitter perspective, goes to make many other molecules including stress hormones and endogenous opioids, the possibility being that too much unrelenting stress could deplete supply and chronic pain problems could arise more easily. Here is a video of that discussion.
Remember the idea that the brain is always busy, always moving, always waving like the ocean.
There was recently a conversation on Facebook about sleep paralysis. It had started going into psychologically deep, potentially mystical explanations about the meaning of dreams and so forth.
I recalled an episode of sleep paralysis I had had, where I dreamed I was fastened to the front of the cowcatcher on a train, heard the roar of the train, woke up terrified and unable to move anything, but finally managed to roll my eyes a little, a small volitional movement but enough to wake up the rest of me. I proposed that it was no big deal, that sleep paralysis was just one bit of brain waking up ahead of some other little bit of brain, sort of the opposite of sleepwalking where one part stays fast asleep while other (motor) parts awaken and fully act out whatever dream state is happening. Squeezing eyelids or moving eyeballs is how I figured out as a child that I could move out of a nightmare.
The brain is not a monolith. It's an evolved organ with plenty of old parts, not just new parts. It's a kluge. It's like the sod shack on the prairies that was simply encapsulated by newer bits until from the outside you see what looks to be a multi-story mansion but if you enter, in the middle of the basement you'll find the old sod shack still in existence and still functional. Nature doesn't usually get rid of anything. If it can't repurpose it, it will just let it sit there like the appendix. (Except it did get rid of tails on us human apes. But I digress.)
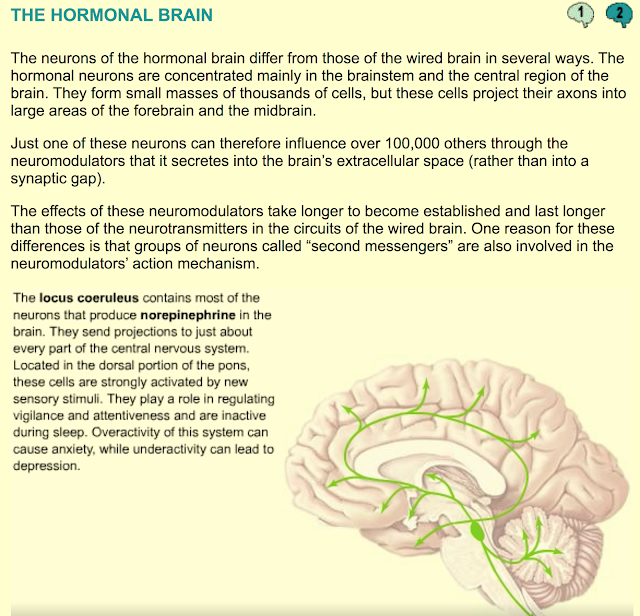
Locus coeruleus ("blue spot") in the brain stem, with only 10,000 cells on each side, is the bit supposedly responsible for arousal and attention focus. It also wakes us up in the morning. It squirts noradrenalin or norepinephrine all over the forebrain. It also squirts it down into the spinal cord which, lest we forget, is still central nervous system and is like the sod shack that was built first before all other improvements came along later. LC wakes up that circuitry as well, is very connected to the sympathetic nervous system which also inhibits ascending nociception at spinal cord levels, very handy if you are a creature all scratched up, fighting for its life inches from the jaws of another creature.
Apparently, LC does not secrete synaptically but rather hormonally, by squirting into extracellular space. How cool is that? It can activate way more neurons that way.
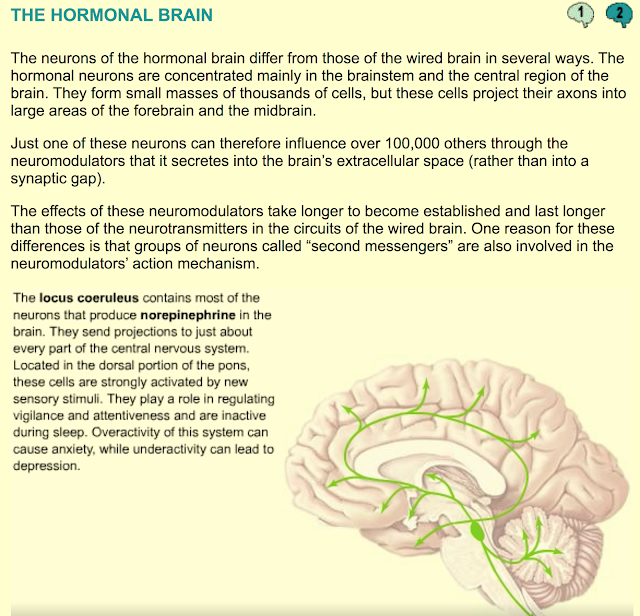
From https://thebrain.mcgill.ca/
So many arguments on Facebook are about whether pain is sensation or perception. I would argue that if chronic pain is a sensation, it's likely going to be interoceptive. And if it's interoceptive, there will be a lot of neurotransmitter involvement and hemispheric cooperation/failure to co-operate, failure to inhibit, maybe opioid deficit somewhere. And if the "I" illusion in there can't feel itself as "normal" because of a very unpleasant sensation, that is going to be a very unpleasant perception of a very unpleasant experience. ..........
1. Tucker, D. M., & Williamson, P. A. (1984). Asymmetric neural control systems in human self-regulation. Psychological Review, 91(2), 185–215.2. Tops, M., Quirin, M., Boksem, M. A. S., & Koole, S. L. (2017). Large-scale neural networks and the lateralization of motivation and emotion. International Journal of Psychophysiology, 119, 41–49.